Concerning Numbers
According to the North Carolina Department of Health and Human Services’ state Opioid and Substance Use Action Plan 3.0, released in October 2021, the number of people receiving dispensed opioids has decreased by 36%, and those uninsured or on Medicaid receiving opioid use disorder (OUD) treatment has increased by 48%, there is “much work left to be done.”
That's been made clear by some grim numbers, including an increase in opioid overdose emergency room visits.

Fatal overdoses also increased during the pandemic — a tragic setback to the state’s mission to reduce these deaths by 20%.

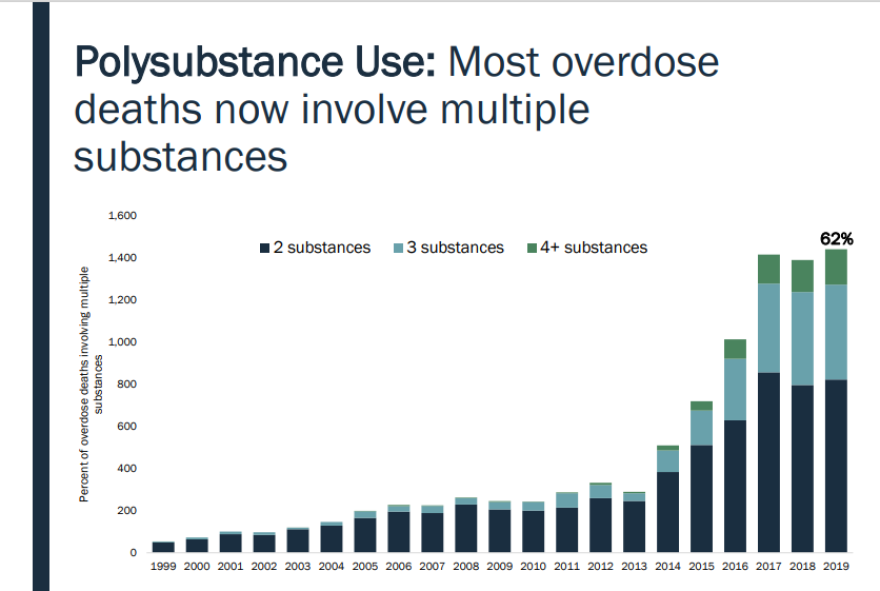
The epidemic appears to be evolving, as well — becoming an increasingly more complicated use disorder as those who are overdosing are using more than four substances. [Editors' note: Some of this may be due to more detailed reporting and documenting but any experts believe polysubstance use is substantially increasing.]
The stigma of opioid dependencies and MAT is still a problem
Dr. Karen Isaacs is a family doctor at New Hanover Regional Medical Center and works at Coastal Family Medicine. She’s also a core faculty member for the family medicine residency program.
She finds that hospital personnel is still dealing with the stigma that comes with a patient having an opioid use disorder (OUD). Oftentimes those coming in with OUD are not comfortable with telling the staff about it.
“They will say to the physicians and nurses, ‘Hey, I can’t be here any longer. I know you’re not done treating my pneumonia, but I got to get out of here,’” said Isaacs.
She said healthcare staff is working on asking, 'What's going on?' in a compassionate way, and then providing ways to treat their opioid use disorder while patients are in the hospital.
That treatment often means offering those patients medically-assisted therapies (MAT) like Suboxone or Subutex. Both at the hospital and at her clinic, she’s able to prescribe — though not dispense — this type of medication for OUD.
But as WHQR has reported, physician prescribers like Isaacs are hard to come by in the Cape Fear Region.
“That can definitely be a barrier. Number one, we just need more prescribers, be it a physician’s assistant, nurse practitioner, or physician,” said Isaacs.
There are two main routes to receiving medications like buprenorphine in the Cape Fear Region. The first is through federally regulated treatment facilities like RHA or Coastal Horizons — these also have the ability to prescribe stronger opioid replacement medications like methadone — and the second is outpatient care physicians like Isaacs.
But the $24 million residential alcohol and drug treatment facility The Healing Place of New Hanover County, set to come online in the fall of 2022, will not allow MAT. Up to 100 women and 100 men who decide to reside at the facility for anywhere from 4 to 9 months will receive non-medical detoxification and support through peer mentors who have gone through the program.
“Housing is definitely a big carrot hanging in front of someone if they’re otherwise facing major social determinants of health (things like access to housing and being employed). I’m not familiar with long-term housing options, other than recovery houses,” said Isaacs.
Isaacs said, “We have tons of evidence that shows that MAT can be incredibly helpful for someone with a history of an opioid use disorder, but if we look at the flipside of someone who has a different way of overcoming that, then why minimize it? Let’s figure out what the patient needs and go with it.”
Those who represent and evaluate the program model of The Healing Place have said one reason for not offering MAT is that it doesn’t address the underlying reason(s) opioids are being misused.
“I don’t think if you interviewed anyone at an outpatient treatment program, that any of us think Suboxone is the only part of someone’s recovery. We almost 100% understand that Suboxone is just there to chemically help with cravings and the physiologic dependence,” said Isaacs.
She said that the way physicians view MAT has evolved over time, too.
“We thought, ‘Oh, my gosh, if we still have them on methadone or buprenorphine in six months, we failed them; we’ve actually replaced one problem with another,'" she said.
But now Dr. Isaacs says more physicians think, “if me taking off their medication too soon is going to lead to a relapse or worse overdose and death, then I would much rather have them on that medication longer to help them sort their life.”
And she added, medical professionals have to be more realistic about where their patients are in the process of their opioid misuse: “Sometimes we forget that patients are sometimes going to do risky things, and if we at least acknowledge that and acknowledge where they are, and in concert with them, offer them a route to reducing harm.”
Helping patients through withdrawal is also another reason to have them on MAT, “So once out of the hospital, they’re thinking straight, they’re not worried about how they’re going to get their next opioid supply to use. They can now think about their families, social situations, jobs, responsibilities, and get to their next outpatient care appointment,” said Issacs.
“I think as from my standpoint, as a family doctor, the biggest thing for me is that we meet people where they are, and as a healthcare physician understanding there’s no quick fix,” said Isaacs.
Tides, Inc. success with MAT
Dr. William Johnstone is a consultant for New Hanover Regional Medical Center and is the founder and president of Tides, Inc, which is a non-profit organization in New Hanover County that supports and provides care for opioid use disorder in pregnant and postpartum women. It’s been in operation since 2018.
He, like Dr. Isaacs, said there’s no quick fix when it comes to helping those with OUD. He said his organization, mainly supported financially by New Hanover County, sees about 33 women a year and houses about 8 of them while they receive treatment.
“So they're being maintained on medications for opioid use disorder, and their prescriber, once the woman becomes pregnant, can refer them to us. And so we take them over during their pregnancy and during their postpartum period until they're stable, and then we can send them back to their treatment program,” said Johnstone.
Over the past three years, Tides has shown some promising results:
“The infants’ stay in the hospital, after being born to a mom with opioid use disorder, is down from 9 days to 6 days. And the length of stay in the NICU has been reduced from 4 to 3 days just by virtue of the fact that these women are now on buprenorphine instead of illicit drugs. And over 94% of our moms maintained some form of custody of their children, which means that before the Tides was there, that number was in the single digits if not zero,” said Johnstone.
He said long-term treatment programs, like Tides, Inc., are the gold standard when it comes to recovery.
“If you come to us and you live with us in our facility, then most of our graduates stay with us from 12 to 18 months, and science proves that the longer a person with an addiction stays engaged in a treatment program like ours, the greater the success for long term recovery,” said Johnstone.
And the science, according to Dr. Johnstone, is clear that most of these women would need to be on MAT: “And we know that women that are on buprenorphine have fewer relapses and fewer overdose deaths, which our ultimate goal is to prevent death. Some women in our program require methadone, and that's done through Coastal Horizons, but I'd say 99% of our patients are on some form of medication for opioid use disorder.”
As for the non-medical, peer-led approach of The Healing Place of New Hanover County, Dr. Johnstone is supportive of what it can do for the Cape Fear Region.
“The Healing Place is going to provide huge resources for New Hanover County. I'm happy to have supported it publicly. And everybody's got a different theory on the treatment of addiction. And abstinence is one of those theories. Again, the treatment is one thing but overdosing and overdose deaths are, to me, unacceptable, when we have ways to prevent that,” said Johnstone.
One of Dr. Johnstone’s former patients, Krista Turner, is now 3-years into her sobriety. She first met him when she ended up at NHRMC for endocarditis as a result of her opioid misuse disorder – and she was pregnant. She spoke to WHQR’s CoastLine in February 2019. Dr. Johnstone shared that Krista's thriving:
“She’s married. She’s got custody of the infant that we delivered, as well as her 14-year-old son that she lost years ago. She’s got two jobs; she just won a car with one of her jobs. She is actually on our board,” said Johnstone.
According to a recent 2021 Harvard Medical School study, as reported by NPRs’ addiction correspondent Brian Mann, roughly 75% of people with addiction achieve long-term recovery, although some experts estimate that it’s a difficult road ahead, that oftentimes people relapse upwards of 5 times before getting better.
So it’s important to Dr. Johnstone that the community does not give up on those in the grips of addiction: “If we can just peel back the onion on these folks – that are family members of ours that are dealing with addiction. Yea, we get frustrated with them because of the lies, the stealing, and the legal issues that come along with it, but if you just peel back the layers, there’s still a soul, there’s still a human being very deep in that troubled mind.”
With the success of Tides in the Cape Fear Region, Dr. Johnstone is in the process of organizing Tides, Inc. of the Sandhills in the triad area.
MAT in the Judicial System
Julius H. "Jay" Corpening, who is the chief district court judge for the 5th district, said he is supportive of the work of Dr. Johnstone and Tides and even has several women on his caseload who reside at the Tides recovery house.
Corpening said he’s strongly vested in the work of Tides, Inc. and Coastal Horizons and the future Healing Place of New Hanover County because the opioid epidemic is "still running amok in our communities."
For him, the most disturbing trend is the flood of illicit fentanyl into the community from China and Mexico.
“Fentanyl is a stone-cold killer. Holy cow. I think I’m just trying to think back over the last maybe six months, I think every person that I’ve seen who overdosed and then was brought back with Narcan, or every single person that overdosed and died leading to their child coming into care overdosed because of fentanyl. It may not have just been fentanyl that they used, but fentanyl was the lethality factor. And I think that the isolation factor for folks who are in recovery is so tough,” said Corpening.
While Corpening doesn't preside over the drug treatment court, he meets with that team regularly, and said, “They've got some of the highest numbers of participants that they've ever had. And so the need is higher than ever for that service. In child welfare, substance misuse continues to be the leading reason for the removal of children from families.”
Corpening said that when these parents end up in family court, they first do a comprehensive clinical assessment of the caregivers to determine the best pathway to recovery for them: “We do have provider choice, but we take advantage of assessments where the person has a voice.”
And that voice involves them deciding what treatment modality is best for them.
“There's an interesting divide in the treatment world regarding opioids because folks who champion abstinence-based recovery are very critical of folks who use medicine. Sometimes folks who use medicine as treatment are critical of abstinence-based recovery and point out the comparatively low success rate. But some folks need one or the other, and if you try to push someone into a treatment regimen that isn't right for them, then you can push that square peg into a round hole all you want, it's not going to fit,” said Corpening.
He added that this process to decide whether MAT or not shouldn’t be an ‘either/or’ but ‘both’. However, Corpening did say that while he’s a fan of whatever works, “I believe that for opioid use disorder, particularly, medication-assisted therapy is the best way to go. The data shows that, but it doesn’t work for some people.”
$750 Million coming to NC from the opioid settlement
On Monday, January 10th, North Carolina Attorney General Josh Stein released a statement that said the state is moving closer to receiving $750 million from the $26 billion multistate agreement with three major pharmaceutical distributors — Cardinal McKesson, AmerisourceBergen, and Johnson & Johnson to pay for their roles in fueling and profiting from the opioid crisis.
Stein also created a website for the state's 100 counties and 45 municipalities, which are set to receive some amount of funding from the settlements.
The attorney general is also mandating that those funds, once received by counties and municipalities, will have to go into a special revenue fund that will be audited. Additionally, local governments will submit annual reports on the funding that will be public via this dashboard.
New Hanover County Manager Chris Coudriet was a member of the North Carolina Association of County Commissioners’ opioid settlement working group, which helped to “maximize the state’s share of the $26 billion settlement fund to ensure resources reach communities as quickly, effectively, and directly as possible,” according to county Chief Communication Officer Jessica Loeper.
In the agreement for North Carolina, these settlement funds may support or fund one of 12 strategies. Second on the list: ‘Evidence-based addiction treatment’ which includes supporting the delivery of MAT like Suboxone. According to the agreement, funding uses "may include capital expenditures for facilities that offer evidence-based treatment for OUD" — it can also be used to partially fund facilities that only offer MAT as a portion of its services.
Over a period of 18 years, (2022-2038), New Hanover County is set to receive $18.6 million and the City of Wilmington will receive close to $770,000.
Loeper said, “the county will work with the city and community partners to identify needs and gaps in services, then develop programs, initiatives and solutions that help people who are struggling with opioid abuse and to help prevent opioid abuse in our community.”
Jennifer Dandron, the media manager for the City of Wilmington, said about the future monies, under the county/city interlocal agreement for these funds, “we will pool our funds with the county to help leverage what we receive for greater overall impact on our community than if we try to use those dollars separately.”
In his opinion, Judge Corpening said “[a]dolescent treatment would be a priority. I think that once The Healing Place has opened we’re going to have a pretty solid response for residential treatment for abstinence-based recovery, but some folks who opt for medically assisted therapy also need residential treatment. And that’s expensive. And if you’ve got insurance, there are places to go. If you don’t have insurance, there aren’t. It’s very limited, so I think that would be a priority for me. We really don’t need another corner store that does methadone.”
Related: April 2021 Statement from Chair Julia Olson-Boseman on the settlement agreement


